Image via Wikipedia
From time to time I get emails from readers with various types of running injuries. Given that I am not a medical doctor, I generally don’t feel comfortable doing much more than discussing the anatomy and sharing some houghts, and usually my advice is to seek professional help if an injury is of major concern to a runner (in other words, I know and respect my limits!).
Sometimes, however, a particular problem can benefit from advice provided by other runners who might have dealt with a similar issue. My hope in posting the following story is that someone who has experienced or is knowledgeable about what Allan is going through might be able to provide some helpful advice.
Here is Allan’s story:
I have been running regularly since 2004. After a long down time with a hip injury, I decided earlier this year that since I was starting from ground zero, I was going to do all of my running either barefoot or in minimalist footwear, mostly Merrell Trail Gloves, but also Vibram Fivefingers KSOs and Bikilas. Before this year I was mostly running in Asics Nimbus, Nike Air Max 360, and Mizuno Wave Creation. During my minimalist transition, I carefully controlled the mileage and intensity buildup, never increased it more than 10% per week, and cut back 50% every 4th week. Very conservative. I gradually ramped up to where I was doing 1 run a week of 4 to 5 miles barefoot and 2 or 3 recovery runs of 1.5 miles barefoot. The rest of the runs were in minimalist shoes. As my long run got up to about 6 miles I started getting some soreness in my left heel near the Achilles tendon insertion. Longest runs were 11 miles before the pain flared up so bad that I had to stop running.
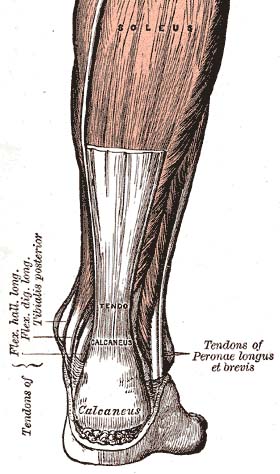
The heel pain started out gradually, went away as I warmed up, and went away the next day. Pretty typical story. It was always better before the next run and didn’t affect my gait so I kept going. But over time it got worse, started swelling, etc. Finally after a 5k on a very hilly course it got so painful and swollen that running was no longer possible. I stopped running and after the pain didn’t go away with rest, I went to the doctor and got diagnosed with retrocalcaneal bursitis. A month of PT and anti-inflammatories didn’t clear it up, so the doctor took X-rays which revealed a Haglund’s defect, which is a large spur of bone extending from the calcaneus just behind the Achilles tendon (see photo below). The doctor recommended surgery to remove it. The spur was apparently digging into the tendon and bursa and causing the inflammation.
Haglund Deformity – note the large, pointed spur extending up from the calcaneus (heel bone)
I have gotten things calmed down enough to start doing very limited running, but it is still uncomfortable. I’m developing a theory of what is going on, so I tested my hypothesis this morning by dusting off my high heeled running shoes. Guess what. Things felt much better. So, what I’m thinking is that over the last several years my heel has remodeled at a particular angle dictated by the footwear I was wearing, which all had traditional raised heels. When I started running exclusively in my bare feet and flat shoes it changed the angle of my foot at mid stance such that the spur was now protruding back into my Achilles tendon and its bursa. I suspect that this wasn’t a problem when I was running only occasionally in my bare feet. But once it was full time my Achilles never got a chance to calm down.
I recently went to another orthopedic surgeon who specializes in foot and ankle surgery and he didn’t recommend surgery to remove the Haglund structure (he didn’t call it a defect). He said that lots of people had it and that it shouldn’t be a problem. He noted tightness of my calves and Achilles tendon and recommended continued stretching. I was already working on this but even doing this irritates the bursitis and tendonitis. I again suspect that it is the Haglund structure digging into the inflamed tendon and bursa.
I’ve learned one thing regarding stretching. I was doing the traditional calf stretch, which stretches the gastrocnemius, and I’m pretty even on both the left and right side and it’s not too bad. I didn’t know about the soleus stretch that is done with a bent knee. I’m actually very, very tight in the soleus on the injured side so that is what I’m focusing on right now because that seems to be what is limiting my dorsiflexion. So, the Haglunds’ seems to be a contributing factor, but both doctors and my physical therapist would concur that my lack of ankle dorsiflexion (only about 7 degrees) is probably contributing as well. I had ligament (ATFL) reconstruction on the ankle in 2008 and that probably left me with reduced range of motion, although I think we got most of it back. However, with the injury it has tightened back up. I’ve had other injuries over the last year and tend to be very tight anyway and I suspect that combined with the barefoot running it may have caused the soleus to get very tight. Don’t know. But it’s very tight and getting things stretched back out is a slow and painful process. So right now the combination of the Haglund’s, tight soleus and AT seems to be a recipe for a really sore heel.
I’m curious about the cause of my Haglund’s – given the size of the spur, I’d guess that it had to have developed prior to me making the minimalist/barefoot transition. When I went for the consult with the foot and ankle specialist he said that a typical cause is repeated rubbing of a stiff heel counter against the heel bone. However, none of the shoes I wear seem to irritate the heel. I’m an engineer so it’s pretty casual wear at work and I always wear running shoes. I almost never wear dress shoes. If anything, the raised heel of my running shoes provides relief by taking some stress off the AT, and probably by changing the angle of the AT relative to the Haglund’s structure. For now I’m going to go back to running in traditional running shoes to see if that will keep me out of surgery, and not lead to a recurrence of my past hip issues. If that successfully rehabs my bursitis then I’ll return to using barefoot running as a tool and run only once or twice a week and not on my long runs. Maybe over time that spur will remodel and allow a more gradual transition to exclusively minimal footwear.
I’m curious how many runners are affected by this and if runners who switch to minimalist footwear are more prone to this kind of injury.
I’m also curious about what those who have dealt with Haglund’s and retrocalcaneal bursitis have done for therapy. Is surgery the best option, or can I manage just by using my high-heeled footwear? Any thoughts on a potential cause in my case? Any advice on how best to proceed?
And finally, I guess a word of advice to those transitioning to minimalist footwear – high heeled shoes can actually help with insertional Achilles pain.
If you have any thoughts or advice, feel free to leave a comment!
















I have Haglunds in BOTH heels. Doc says it is a genetic structure thing. When trying to convert to minimal drop shoes it got really irritated so i went with a bit “less shoe” and use my custom orthotics that give me a bit of heel lift. Keeping my calf and soleus loose is a big key.
I don’t have any advice, and I don’t have the same issue… but I do have a comment:
You left out one of the most important bits of information: a video of you running.
Minimalism or barefoot running is not a goal in and of itself. The point of minimalism is that it should offer the opportunity to improve your running form and, with better form, you should be able to run without a problem.
Does that mean that minimalism/barefoot is the answer for everyone. Maybe not.
But, again, my point is, we don’t have enough info from your post to see which “camp” you might be in.
I have seen WAY more than my share of runners who’ve switched to barefoot/minimalist and have not adjusted their stride much, or at all. Or, they’ve adjusted it dramatically, but not to become more efficient (kicking their feet out in order to land on the forefoot, trying to stay on the ball of the foot without letting the heel drop, etc.). And, none of these runners ever knew they were doing something that put them at risk for injury.
So, once again (and I’m only repeating this, ad nauseum, because when I make this point it’s often mis-understood), we have to be careful not to confuse being barefoot/minimalist with either a cause (or cure) of a problem unless we have all the details at our disposal.
Sorry, no video. But I was a heel striker in my old running shoes and I know that there were definitely weird things going on in my gait that I suspect contributed to the hip injury that kept me sidelined for most of 2010. I’m definitely forefoot striking now, not heel striking, and being a big guy it required a very slow and deliberate transition. I started out walking very short distances and ramped up the distances very, very slowly. I did it barefoot and the soles of my feet did a very good job limiting the distances for me and giving me feedback.
I’ll have to see if I can get my son to take some video of me running barefoot and in my running shoes. I honestly have no idea what I look like running. I just know what it feels like. I’ll shoot some video and post it and you can tell me what you think. Try not to laugh too hard. I’m kind of built more like a linebacker than a runner.
Wow. I’m living through a similar story, but not as far along as you. After running the Mt Desert Island Marathon (which I highly recommend) last October I had to take six months off due to a “sports hernia,” which I ultimately had surgically repaired. Before this, I was running about maxing out at 50 miles/week with about 5-10 miles in VFF (most of the rest in LunarRacers). Like you, in starting again from scratch, I’ve done almost all my running in VFF, Trail Gloves and Inov-8 XRoad 155. I’ve successfully focused on my gait/cadence and have very slowly — over four months — have worked up to 20 miles a week. But over the last month or so my left achillies, about 1-2 cm above the heel, is sore much of the time. It doesn’t get worse as I run or play tennis (competitively) and doesn’t limit my activity, but I notice it and worry I’m aggravating the injury. An orthopedic surgeon friend of mine examined it (no x-rays) and dismissed the injury as typical achillies tendonicity — take it easy and let him know if it gets much worse. I don’t want to stop training but plan to take the next 7-10 days off to see if that will give it a chance to settle down. While I stretch after runs, I don’t do it as consistently or intently as I should. Perhaps that will help. Thanks for sharing your story and learnings. Good to now others are struggling through similar experiences.
Hi Pete & Allan ,I had Haglunds & found relieve sleeping in a Coriflex medical boot .It maintains dorsiflexion whilst sleeping .I suspect this may have happened due to lax ligaments from your ankle injury . I went on to run a marathon 3 months later .Also check out Dr Hauser @Caring:disqus Medical.com .
I now have a torn Meniscus Dr Hauser is giving me Prolotherapy & PRP .My surgeon said I probably wouldnt run again Dr Hauser said I will .This was a few weeks after Boston ,not what you want to hear .He is an Ironman & Boston Marathon runner in Chicago .Please look at his website .I am sure he can help ! Good luck .
I’d say from the info you provide, a lot of your problem is from the footwear and past injuries, and maybe even toss in a bit of overtraining. Past injuries cause major adaptations in the body and even though the pain may be gone, gait imbalances and muscle imbalances are still present. I’ve got a Sock Doc post and video on Achilles Tendonitis – retrocalcaneal bursitis – pump bump; call it what you like, they’re all names given from a similar problem. link to sock-doc.com…. From my experience – stretching and orthotics are two of the worst things you can do for that, as well as most injuries.
I’ll add my thoughts here. It’s important to keep in mind that Achilles tendinopathy is not a single condition. Pain higher up in the tendon probably results from a different cause, and would require a different treatment approach than the problem described in this post (eccentric calf exercise is a common treatment approach for pain higher in the tendon).
In this case, the problem is being caused by a big hunk of pointy bone that shouldn’t be there. Personally, I don’t think this is a case where being dogmatic about minimalism or barefoot, or even necessarily running form, is all that helpful. The issue is that a pointy hunk of bone is digging into the bursa and tendon when the tendon is angled a certain way relative to the bone. The solutions are either to remove the bone spur, or find a way to avoid the digging. It seems that in this case, a heel lift angles the tendon relative to the bone in a way that alleviates the pain. If that allows you to run, why not go with it? The issue though is the past hip injury, so determining if that might be related to form/footwear could be of interest.
My guess is that when the foot dorsiflexes during stance it causes the spur to impinge on the bursa/tendon as the tendon forms a more acute angle with the calcaneus. Similarly, I suspect excessive plantarflexion in a shoe with a stiff heel counter could also be problematic as the heel counter could push the tendon from the backside forward against the spur. This would explain why running the 5K on hills was so painful – hills probably accentuate dorsiflexion on the way up, and plantarflexion on the way down.
Given this, my suspicion would be that a shoe with a heel lift and fairly soft and flexible heel counter would be ideal given that the spur is already present.
Now, the other question, and the more challenging one to answer, is how the bone spur got there in the first place, and whether it would come back if it were surgically removed. That’s where I’m at a loss right now.
It’s kind of a catch 22 for me. I felt like the barefoot running was really helping me run much more comfortably and for the first time in over a year I was running without hip pain. It was wonderful. However, the new running for definitely put more stress on the lower leg. I was very conscious of that and tried very, very hard to not commit the mistake of too much too soon. However, I still wound up with the heel injury. So I’m wondering there really are some factors that prevent some of from being able to run barefoot or minimalist. Whether it’s the Haglunds, the lack of dorsiflexion, or both, running in zero dropped shoes or barefoot hurts my heel.
The minimalist shoes you mentioned are all zero drop. Have you tried anything with an intermediate heel height that might help your hip and still avoid the heel pain? Maybe something like a Nike Free Run or Saucony Kinvara? Both have fairly flexible heel counters.
Pete
Sent from my iPad
I have the Kinvara and some lighter racers/trainers. That is the route I’m going with for now although it is frustrating. I really liked running barefoot…
Allen, I had my Haglund’s defect surgically removed about 15 years ago, but it has grown back by now. The rehab was a real PITA. I started running back in 2009 mostly in Newtons which have a lower heel-to-toe drop (5-0 mm). I found that zero drop shoes or tighter racers definitely cause more problems for me. I am not to the point where my dress shoes are frequently cause inflammation but it does happen. Body glide might help reduce the friction / rubbing. Currently, what works best for me is icing to keep the inflammation at bay.
I am curious if you are still running in Newtons and if so, do they help keep the inflammation of the Hanglund’s bump at bay? I have had the condition for 10 years now. I have had several severe flare ups that have required a couple weeks off to calm things down. Yesterday, during a hilly half marathon, I suddenly had a lot of pain in my heel and ended up limping the last 4 miles to the finish. This is the worst it’s ever been. I think it’s just acute inflammation (as opposed to having ruptured or fractured something) but it’s so painful. Normally after a few steps, I can walk without limping even when it’s flared up. I can’t do that today. I am beyond frustrated and am trying to decide if I should make the switch to a more minimalist type shoe like Newtons, or maybe Pureflow by Brooks. I have always thought that the further down my heel sat in a shoe the better it would be because it would be less friction. Now I am starting to wonder if that position is causing more stress on the area. I have been thinking about Newtons for awhile and as I sit here on the couch with an ice pack wrapped around my foot, I wonder if I should just take the plunge. I won’t be running for at least a week because I have to let things calm down but maybe it’s time to experiment. I thought perhaps a shoe that was encouraging a midfoot/forefoot landing would take some pressure off the achilles. Would love to hear your thoughts and shoe experiences.
Thanks! Debbie
Hello Allan: As you’ve found out (the hard way), these aren’t easy problems to treat. They take a different bend in their treatment as compared to achilles tendinosis problems due to the nature of the Achilles enthesis, which (per recent research) is much more complex and layered in structure than was previously understood. Certainly, you have to handle these problems gently – it’s not as vigorous an approach over the long run as is typical with Achilles tendinosis (using an Alfredson protocol of eccentric emphasis heel raises), although I’ve found that you have to pursue that route eventually, once you establish a baseline of how much activity it takes to provoke the heel pain.
You mentioned your size – how tall are you and how much do you weigh? You also mentioned your ankle/achilles inflexibility – the degree of motion you noted (7 degrees) is marginal, even for shod running, much less for barefoot. Lots to look at there alone, including whether your lack of mobility is truly gastrocnemius, soleus, or just lack of talocrural mobility – those are things that your PT probably has figured out (both by measurement and by looking at your functional squat ability), but you need to aim for 30 degrees of dorsiflexion , particularly if you’re trying to train using a minimalist approach, along with 1st toe dorsiflexion flexibility. Deficits in these will show up in a video exam of your running form.
Other things to consider – I often find that I have to do “surgery” on heel counters in the training shoes in those runners I treat – some shoes are worse than this than others (such as Saucony’s Fastwitch 4) – pulling down the upper off of the heelcounter and trimming down the back of it – some shoes require just plain cutting off the heeltab, as any pressure that presses on the achilles above the insertion will cause more problems. Some will recommend against using deep friction techniques on the enthesis, but I’ve found success with Graston techniques for lessening the local symptoms. Careful kinesiotaping helps with the symptoms as well. These are the band-aid things, but addressing the mechanical /soft tissue deficits from foot up, making sure to deal with any restrictions in talocrural and subtalar mobility and any form issues and stance control both balance and calf endurance) issues become more important to resolve this. Your return to footwear to control the pain for now is smart – whether this will really cause the spur to resolve (i.e. Wolff’s law) is probably more conjecture than anything at this point.
Kent,
Thanks for chiming in! Does the impingement of the spur against the bursa tend to occur more in dorsiflexion, or during plantarflexion as a result of the heel counter pushing the tendon toward the spur from behind? Also, is this mainly a sagittal plane issue, or does ankle inversion/eversion play a role as well?
Pete
Hey Pete – good to talk to you! Really, these can go either way (or even both) in terms of impingement. The thinking of the mechanism/purpose for the retrocalcaneal fat pad is that it acts akin to the patella as a soft fulcrum to improve the leverage of the achilles for plantarflexion. Any bony development, though, tends to produce kinking against the tendon and instead of a smooth distribution of pressure over the enthesis, point loading occurs that increases the tendon stress.
None of these problems are purely sagittal plane – you have to look at pronation/supination. Most of the time (as Allan noted himself), the original symptoms often occur on the medial side of the tendon – poorly mediated pronation causing the stress on the side of the tendon (the convexity) most under stress during stance. I often find that runners with these problems have a forefoot varus alignment, even if their rearfoot alignment is relatively normal during stance. Barefoot video analysis shows this well and I find that more reliable than trying to accurately bisect/marker the rearfoot and lower leg (though I still do so as best I can).
My own 2-cents opinion, for what it’s worth- Surgery isn’t necessarily a bad option with these, as long as you resolve the mechanical factors that led to the original spurring. Orthotic intervention can help as well if there’s either rearfoot and/or forefoot motion that appears to be driving this, although that’s not necessarily what a minimalist runner wants to hear. I’ve found that for runners wanting to go the minimalist route (short of barefoot) that you can sculpt a “cobra pad” for shoes such as the NB Minimus and have that work well to lessen the mechanical stress of pronation without mucking up either the shoe or minimalist training (link to jospt.org….
In regards to the eccentric training approach, Alfredson has addressed the issue of this in regards to insertional enthesopathy (2008) – he claims a 67% success rate in the sample of 27 of their study – the abstract for this one is on BJSM – food for thought, though it doesn’t take into consideration the impingement/spur issue.
Thanks for the info Kent. The other option I was thinking would be to simply get the lightest shoe possible with a traditional heel lift, and as you suggested, slice out the plastic heel counter (if present). Something like the Brooks T7 Racer or New Balance MR1400 might do the trick. This way you can at least reap the benefits of a lightweight shoe.
Another option might be one of the Tri shoe with the elasticized heel counter, something like this perhaps: link to scott-sports.com….
To me, this is a case where you do what works to alleviate the pain – if that’s orthotics or a heel lift, then so be it. If I were in this position that would be my first line of attack before going the surgery route. Again, though, it’s critical to figure out what caused the spur to form, and to know if it might continue to grow if you maintain a more conservative approach.
Pete
I’m 6/2″ and 230 lbs. and about 22% body fat. My background athletically is wrestling and bodybuilding, not running and my legs are very large and muscular and not very flexible. On the leg press I do sets of 8 with 720 pounds. My thighs are currently 26 inches around and my calves are 17 inches. They’ve shrunk a lot since I started running but are still pretty good sized. PR in the marathon is 4:17 and in the 5k is 23:36.
My heel pain was initially at the enthesis on the inside of the heel. That pain was/is moderate. The severe pain and swelling actually came from the bursitis and flaired up later as the symptoms progressed. I don’t really have any tendon pain higher up in the body of the tendon. After 3 months of rest and a topical medication from my doctor the bursitis seems to be pretty much gone. Poking around on the heel the pain seems to mostly be at the enthesis on the medial heel.
I have pretty good dorsiflexion of the 1st toe. PT didn’t indicate any problems there.
One question I have on measurement of dorsiflexion is how it’s measured. When stretching I have no problem achieving pretty good dorsiflexion of both ankles now. However, the way that the PT measures dorsiflexion is sitting on the table and pushing on the ball of my foot with his hand. Frankly, my calves are never going to allow anyone to push my ankle to 30 degress of dorsiflexion with their hand. I might be able to easily achieve it standing and leaning forward, but it isn’t going to happen sitting on the table like that. I’m just not sure whether the guidelines and method of measurement work for someone with with above average legs. To give you an idea, when I do leg presses I do reps of 8 with 800 pounds.
As far as shoes irritating it, it hadn’t been a problem in 7 years of running. It was actually running barefoot and in minimal shoes that caused this to blow up so I don’t think it is a case of footwear irritating the heel. Even now, if anything the heel lift of shoes relieves symptoms and I don’t feel any pressure from the heel counters.
This sounds exactly like what I have. I had pain in my Achilles after switching to Fivefingers so bad that I could not run. I initially went to a chiropractor for Active Release Technic (ART). This helped a little, but not much. I then when to another chiropractor for Graston Technic. This worked miracles. I was back to running after one session. I went to him weekly for about 2 months, and still go bcd occasionally. I know rest would really help me out a lot, but I don’t plan to rest until I am done with my next marathon in November. The pain is worst first thing in the morning and right at the beginning of runs. One thing that does help is I often wear New Balance Minimus for my long runs. The hill lift is only 4mm, and this really seems to minimize the stress put on the Achilles.
I’ve obviously decided to take the conservative, non-surgical approach to treating my injury, but I originally contacted Pete because of curiosity about the Haglund’s aspect of this injury. If the conservative approach doesn’t work then I need to understand the Haglund’s, what causes it, and whether surgically removing it is going to cure my problem.
It’s somewhat concerning to me that my normal sports medicine doctor recommended surgery to remove the spur. Another foot and ankle specialist recommended by another sports medicine clinic thinks it’s not surgical. My cousin who is a podiatrist has done surgery to remove Haglund’s defects and my google searches has shown that other orthopedic surgeons remove Haglund’s defects to treat this kind of injury.
Being an engineer and being curious I wonder how many runners there are out there with Haglund’s spurs who never have any symptoms. If that’s the case then that would be a good thing to know because it might mean that there are people out there getting unnecessary surgery to remove the spurs when they aren’t really the root cause of the problem.
But I’m also curious about why the develop, who gets them, when, what influences their size, structure, etc. If they really are causing symptoms in runners then that kind of information would seem to be important. Perhaps there are other aspects of the spur that cause them to become symptomatic in some people, but not in others.
I reccomend that you stop doing all your calf stretches, as the latest research on this injury indicates that stretching will make it worse.
Get your physio to release your calves and AT manually, ice the area at least once a day (at night), and apply a topical anti-inflamm r
I have subscribed to this blog for about a year. At times I have almost unsubscribed to it because I was told by my orthopedic doctor this summer that I should give up running. I saw this post and for the most part, this is me. I have a huge bone spur on the back of my ankle. I have had it for quite some time, but it has never really given me trouble. I am a life-long runner and I have just turned 55 years old. My sons gave me minimalist running shoes for Christmas, and I loved them. I built up slowly and once I got used to them, I found that I was running faster than ever. In May, my Achilles tendon began to hurt, it was sore to the touch, so I really cut back on my running. Once school got out in June (I am a teacher), I went to my family practice doctor who recommended an orthopedic doctor who specialized in foot and ankle problems. He did an MRI, and he told me that I have Achilles tendonosis, not tendonitis. My tendon was thickened and calcified. He told me that I shouldn’t run, and that if I had surgery to repair the tendon, and to remove the bone spur, I still shouldn’t run. Needless to say, I was crestfallen. This was the day before my 55 birthday. Running has always been a part of me, and this was not what I wanted to hear. I bought a bicycle and have been cycling, but it is just not the same!
I have not decided yet whether to have the surgery. I will be basically out of commission for six weeks, then in a walking boot after that. Has anyone else experienced this type of situation?
It may be worth looking into shockwave therapy for that Achilles tendinosis problem. It is a fairly new therapy and has shown some good results. If I were you I would first try out non-surgery options to see if they work, and only have surgery as a last resort.
Thanks for the info. I will look into it…have you done this therapy yourself?
I will in a couple of weeks, I’ve got times booked today. In this case it is however for chronic problems in tendons in my forearms (keyboard all day and kayaking all night did not work out). I do have some problems with my right Achilles tendon, but not so severe and I’ve been able to control it with eccentric training programs so far. I’ve had longterm problems in other tendons too (I seem to be prone to such injury), and wanted to try out shockwave therapy earlier after reading about it, but no therapist close to where I live have had such a machine until now.
I booked a meeting with a physical therapist at the health center I knew had bought such a machine, and I never had to ask for shockwave therapy, I just described the problem and she made some tests and then suggested to book a series of treatments. They run 5 treatments spaced with about 5 days as a starter, which may be all you need.
The problem with tendinosis is that the body has “healed” the tendon during stress so it has gotten into a chronic poor state. The body thinks that the tendon is healed just fine so it just leaves it in that state. By firing shockwaves on the tendon part of the structures break down and the body is triggered to re-heal the tendon, hopefully into a good state.
As with all treatments, it works for some and not for others. From what I’ve read so far shockwave therapy seems to be quite successful, moreso than similar treatments like ultrasound and laser.
If it works well for my forearms and I have continued problems with my Achilles tendon I’ll probably try out it on my Achilles too. Here in Sweden therapists are still generally very anti-minimal concerning footwear, so it is not so fun going there with a “minimalist” injury, my Achilles tendon problem is probably due to too much too soon of zero drop shoes. I just want help to overcome the transition threshold and continue down the minimalist road, but I know the therapist will think I’m an idiot and recommend high heels and orthotics :-).
What we don’t know is how many people have the Haglunds deformity and are asymptomatic. And are the asymptomatic b/c they are biomechanically sound everywhere else? How would you know you had one if you didn’t have pain? Are there studies on this? They say heel spurs aren’t the source of pain on the bottom of the foot. Is this the case, too?
I understand what you are saying about the Haglunds deformity compressing the bursa/achilles. Do you have the deformity on the other foot? If your achilles/soleus is tighter on that side, then yes, I can see how the bursa and be compressed between the deformity and the shoe. AND, your body may be compensating and forcing more dorsiflexion in that ankle due to problems elsewhere. Remember your body will move around the path of least resistance. It moves around restrictions and obstacles.
However, if the pain is NOT from the deformity, then stretching can also make it worse. Have you had a diagnostic ultrasound done?
My recommendation: My suspicion is that you have a restricted fibula, which will cause reduced dorsiflexion. Get that checked out. Get a video analysis done. You didn’t mention anything about any hip restrictions or pelvic stability issues. Common issues I see with Achilles injuries is 1) tight psoas/rectus femoris causing increased hip flexion/overstriding and restricted hip extension. 2) Decreased hip internal rotation, causing a cross-over strike, which will cause the foot to land MORE supinated and then “WHIP” down into pronation, in effect, whipping the achilles. Also, sometimes we see poor pelvic stability, causing the cross-over strike.
Lastly, get your cadence to 180. The less time your foot is on the ground at a given moment, the less the tissues have to strain to absorb the impact. Try also to drive your knee FORWARD, not up. This will bring your heel closer to your butt on the swing phase and make you land more underneath your body and not overstriding. Worst thing you can do is let the lower leg swing forward early, extending your knee causing you to overstride and heel strike.
BTW- Heel striking is not necessarily bad- depends on where your foot lands in relation to your body and if your knee is extended or not. Most elite marathon runners heel stike, but its when their leg/hip is already extending, not at the moment between moving forward and then backward (braking). It’s like they are running on a treadmill.
Rarely are injuries caused by a single biomechanical error. It usually takes 2-3. Your body is REALLY good at cheating and compensating, but to a point. Soft tissue can only handle so much then after a while, when pushed over it’s threshold, it becomes injured.
Hope this helps!
It seems unlikely to me that overstriding would be the issue here. He was asymptomatic until he started running barefoot and in Fivefingers, and if anything I’d expect that running in those would have prevented serious overstriding. Pain goes away in shoe with a traditional heel lift.
When I look at the x-ray provided, I see a Haglund’s deformity, but no bone spur. I’m wondering if the terminology and descriptions used here are correct (please correct me if I’m wrong). It’s my understanding that Haglund’s deformity is a radiographic diagnosis, describing an enlarged bursal projection of the calcaneus. The Achilles inserts on the middle third of the posterior aspect of the calcaneus. Traction on the Achilles insertion will cause a bone spur at the insertion (in the middle third of the posterior aspect of the calcaneus), whereas the Haglund’s deformity is not a bone spur at all. Rather, it’s just an anatomical variant. Whether it’s symptomatic or not could be a matter of training volume/intensity, calcaneal inclination angle, and other biomechanical factors such as forefoot varus or equinus.
Heel lifts and cobra pads are simple, can fit in minimal shoes, and could provide relief while you find a way to increase ankle dorsiflexion without further irritation of the Achilles insertion.
I’ll take any blame for calling it a spur, mixing medical jargon and commonly used descriptors I guess :)
Phil,
My understanding is that there is a reasonable chance of recurrence after surgery to remove a Haglund deformity. This would suggest to me that this might be more than just a variant, and that force application in some way is stimulating bone deposition in this area of the calcaneus.
Pete
Thanks, Pete. Good to know. Do you know what the recurrence rate is, and what procedure was done? There are different ways of approaching the deformity surgically, detaching and reattaching the Achilles, and there are some newer fixation methods that might improve outcomes. Just curious.
Phil, don’t know stats on recurrence rate. Just have read it a number of times while poking around on line. Pete
Sent from my iPad
Phil,
This paper does not cover recurrence rate, but indicates 80%+ percent of patients having the type of surgical procedure would choose to have it again: http://actaorthopaedicabelgica…
Pete
Phil S, my understanding is that a Haglund’s deformity is a retrocalcaneal exotosis, rather than an anatomical variant. The bony growth develops following chronic irritation caused by the heel counter of shoes. As you say, this is different to an Achilles enthesophyte. Haglund’s deformities tend to grow because they increase the irritation caused by shoes, leading to a vicious circle. They can be asymptomatic in early stages, but if they grow big enough to interfere with footwear or impinge on the Achilles tendon, they will cause problems.
I got an email from a sports medicine doc who said he often sees them in hockey players due their stiff skates. This would support the chronic irritation mechanism.
Sent from my iPad
Wow, does THIS hit home (thanks Mark U. for the heads-up, and thanks to Pete for this post). Very informative comments, too. I’ve suffered from Haglund’s Deformity for well over a year now. I’ve been an on-and-off runner since 1983, with numerous injuries along the way. I finally got past a chronic IT band problem and, in 2009, started running again. At the end of ’09, I started ramping up my mileage significantly to prepare for my first marathon (May 2010). Shortly after the marathon, I transitioned to trails, hoping to run my first trail ultra in October of 2010. During most of last year, I also worked on landing more mid-foot (I’m still working on getting my cadence up to 180/minute). Anyway, my ultra plan was put on hold, as my right heel started hurting significantly (especially after hilly runs). I went to two different doctors (first a PT, the other a Sports Med doc) before x-rays and an MRI finally showed the source of the pain. I was told it was a genetic condition (my rt heel has dug holes in the backs of my shoes for years), enhanced by overtraining and, as the PT witnessed via video gait analysis, some running form issues. I also have scar tissue built up in my Achilles tendon due to the friction from the Haglund’s Deformity. I quit running, spent a few weeks in a walking boot, and gradually started eccentric heel raises. The Sports Med doc I was seeing was very conservative in his approach, and wanted to avoid surgery unless nothing else worked. I started a walk-run program earlier this spring and have now built up to running 3x per week, no more than 3 miles at a time. I also started using custom orthotics in my regular shoes and running shoes. Back to the video analysis: I pronate more with my right foot than my left, and it appears this is caused by a hip alignment issue (I tend to swing that leg around slightly as it comes forward. I believe a comment here by a doctor explained well what I tend to do). I’ve been doing stretches and strengthening exercises for my hips, glutes and core.
I quit seeing my Sports Medicine doc a couple of months ago, since every visit had become identical. I’ve since been told of another local doctor who uses the Graston technique, and works more with the patient on body alignment issues than my previous doc. I’ll be making an appointment with him soon.
As for stretching, I was told not to do traditional weight-bearing calf/Achilles stretches, but to do them seated using a towel to flex the foot. Well, I’ve started doing some very minimal traditional stretching, just because I’m very tight in the calves and Achilles.
Oh, I meant to mention that I have NOT really run in minimalist shoes. My workhorse the last 2+ years has been the Brooks Defyance models, and I usually race in the Brooks Launch (I’m a Brooks ID member); both considered relatively neutral shoes. Years ago, I was incorrectly put into heavy Brooks Beast shoes (I’m a thin and light guy), which led to IT band problems. The Defyance and Launch suit me better (minus the heel problem, of course).
I’m not sure if I’m adding anything of interest here, but this has been a long and frustrating journey. I hate to hear of others going through the same thing, but I guess it is good to know I’m not alone. I hope we all overcome this roadblock soon.
Like Coach Kevin, I also have Haglund anatomy in both heels. Thanks to other biomechanical issues, I ended up with retrocalcaneal and subcutaneous calcaneal bursitis five years ago. My podiatrist mentioned the Haglund’s casually and that was it. Instead of risking tendon rupture with a cortisone injection, he instead injected Traumeel (a homeopathic antiinflammatory that includes Arnica) for the bursitis and prescribed orthotics with heel lifts. Including the usual running shoe heel lift, I was running in over 2 1/2″ heels. My bursitis went away but my Achilles and hamstrings significantly shortened!
Two years ago, after gradually grinding down the orthotic heel lifts, I dumped the orthotics and inserted an aftermarket insole (1/2″ heel lift) into my Brooks Cascadias, then removed that after about 6 weeks. Then I transitioned to minimalist shoes about a year and a half ago. Like Allan, I too had Achilles pain, a deep grinding pain on the lateral aspect of the tendon. I backed off with my Five Fingers, used Hoka One Ones, which have a 4mm heel lift, and alternated every other run with my Brooks Cascadias, which I think are 12mm. My Achilles gradually lengthened and I dumped the Cascadias.
Now I only run in minimalist or “natural” shoes with 0-4mm heel lifts, including Five Fingers, Merrell Pace Gloves, NB Minimus, and Hokas, because I find regular running shoes give me hip and SI joint pain. The only time I get Achilles pain now is if I wear the Merrells longer than 2 hours, because they have very poor heel anchoring. They rub my heels and since my heel keeps coming out of the shoe, my ankle gets stressed.
I’ve found the most effective long-term strategy is post-run soleus stretching and rolling out the Achilles tendon and calf regularly. That keeps everything calm and problem-free. It allows me to run ultra distances in these shoes, so I’d say it’s working for me :)
Good luck Allan!
Hello! I’ve enjoyed
reading your blog for some time, and as a “new” blogger myself, have used it as
a learning tool. That said, Allan’s
story is a familiar one. I am a
Certified Athletic Trainer, and I’ve treated athletes of all levels, from
recreational to Olympic level, for the past ten years. I should also toss out the disclaimer that it’s
difficult to make general recommendations, as every athlete has a unique
biomechanical structure, and it’s been my experience as a clinician that unless
I am in the same room with said athlete, my thoughts are generalizations rather
than specific, so may vary unless my physical findings tell me differently. In a perfect world, I would love to see his
gait, walking and running, and evaluate a number of items, including his foot
type, both standing and sitting.
That said, it makes PERFECT sense that high heeled shoes
would eliminate his pain, as it positions the foot in a plantar flexed state,
thereby taking substantial pressure off of the Achilles tendon and more
importantly, creating what is known as an open packed position which creates
more space within which soft tissue can “move” without further impedance. When I teach this concept in courses, I use a
slinky as a teaching implement. A
compact (closed packed) slinky is a small, rigid area. You can only fit so much in it’s finite
space; however when the slinky is stretched (open packed), you can fit
substantially more in it’s more infinite space.
Another way of thinking of this
is that when the foot is fully dorsiflexed, it is in a closed pack position
(stretching the posterior musculature and further annoying the tissue). Simply
changing the foot and ankle in a different position of a few degrees can
dramatically change how that tissue interacts with it’s structural “neighbors”,
if you will.
Working up the kinetic chain, I’m curious how the
musculature surrounding his hip is; that is, deep tissue work on the gluts
(specifically the glut med) may free up some motion, creating more freedom of
movement below. He states he had a hip
injury with lots of down time; in his case I would go right to the SI joint and
assess both pelvic structure and soft tissue surrounding it. It’s very possible further work here is
needed, and may possibly be limiting his overall management of the Achilles/et
al. issue. Of course, the only real
problem left is the Haglund’s deformity, which presents substantially and other
than surgery, will be omnipresent. I
agree with his self assessment of continuing to wear traditional running shoes;
this can only help, not hurt. As we are
learning with stretching, it’s not good to always “stretch” tight or sore
structures; in fact, when done to excess, it impedes healing. It’s also possible he may need a longer
period of rest (I know, I know, it stinks, but is sometimes quite necessary)
and more aggressive therapy well above the injury site.
As for retrocalcaneal bursitis or “pump bump” as it’s
commonly called; you do want to limit the friction caused by shoes. That is, it may not hurt while you are in the
shoe, but if it rubs too much, over time it will lead to the area becoming
agitated. It does present a bit of a
conflict: wear loose shoes while running!
I know, this flies in the face of what you are looking to do, but some
ways to subtly change this are to lace your running shoes in reverse; tie them
down near the toes and keep them a bit looser near the eyelits close to the
ankle. This may help. Or, wear your
shoes looser during the day when you are not running, thereby limiting the
amount of time your heel is in direct contact with the counter. If you are at a desk job, straighten your knee
a bit, and allow the foot to rest in a more open packed state (plantarflexed,
toes pointed down). Doing this a few
hours each day may help balance out the time you spend dorsiflexed (standing,
walking, running). Orthotics may help,
but it’s been my experience that most of the time, they don’t. You might be able to try a heel lift in the less
structured shoe.
So, just my initial thoughts as he tries to keep surgery as
a last option. At any rate, hope this helps a bit; and if anyone would like,
you can check out my blog http://www.essentialatc.blogspot.com
You’ve done a great job describing the signs and symptoms of insertional enthesopathies such as Haglund deformity. There are cases associated with underlying arthropathies such as reactive arthritis (formerly Reiter syndrome). I think your approach to it has been a good one. Certainly, a conservative approach initially is the right choice with surgery as a later option if need be. The spur or osseous protuberance is likely the result of bone remodeling according to the pull of the achilles tendon. The problem then is one in which the bursa and tendon are continuously irritated by the protuberance. Surgery can alleviate the osseous abnormality but be aware that the bone prominence may recur and you may experience the same symptoms post surgery.
Allen,
With Haglund’s in both heels and a 20 year history of intermittent heal pain relieved by various efforts at stretching and ice, over the past 2 years Astanga yoga (look it up in Wikipedia) has been the best solution for me. At 55 I am now not only running well, but also moving without pain (eg going down the stairs) upon awakening in the morning.
Running causes the flexor muscles to shorten. The solution is to lengthen them (ie NOT surgery). Sports physical therapy is like “baby yoga” in that for me, it was a bit helpful, but not sufficient. Also it is very expensive.
Three to five hours per week of this intense Astanga yoga has gradually but significantly increased my flexibility, particularly in my hips, hamstrings, and calves. When all these areas get tight, the weakest area breaks down, the Achillies.
I’m fortunate to be near a yoga studio that opens at 5:40 weekdays (“Mysore” class, Yoga East, Louisville, KY) so I can get my routine in before work. Otherwise I don’t know how I could fit this into my day.
As I get older my tight old body just seems to be getting tighter. I’ve signed up for a yoga class and I’ll see how that goes.
Funny, I just put up a blog post about mid-tendon Achilles tendinitis/tendinopathy las week. http://runningwritings.blogspo…
In my post, I go over Alfredson’s eccentric heel drop protocol for Achilles tendonitis, which is quite successful. The protocol was designed for mid-point Achilles tendonitis, but is not as successful with insertional Achilles issues. However, a variant of the eccentric heel drop that targets insertional Achilles problems has been devised and described by Alfredson in this 2008 article: link to msscentershop.info… The only differences between the “classic” heel drop and the new heel drop for insertional Achilles tendonitis is that the exercise is done on a flat surface, and there is no bent-knee variant.
Seeing this post makes me want to write up an update for my own Achilles tendonitis post covering how treatment changes for insertional vs. mid-point tendon issues.
—John
Good article. I’ll try the flat protocol. My tendinitis is much better. My main problem is that the bursitis keeps flaring up I try to return to running.
I am currently doing the heel drops on a flat surface, it seems to help, I am only on my third week. I still have the problem, but will persevere. I did the drops off a step one day, and was in more pain the following morning so have gone back to the other one.
As a general comment, it would be interesting to know how many people that get Achilles problems when moving to zero drop. If I would make a guess, that would be the most common injury problem for newbie minimalists. I wonder how many that is forced to stop their transition due to this type of problems.
I have also been troubled by one of my Achilles tendons since I started with zero drop shoes in daily life and in running. Not as serious problems as described here, but certainly has stopped me from running in periods and is currently a limiting factor.
Another sufferer here… I have had insertional achilles pain since I was in high school. I have haglunds and protusions so big on the backs of my heels that I eventually wear deep pockets to accommodate them in every pair shoes I own. In 2005 after I raced in a series of 5k/10k races, it got so bad I had to stop running. I was told by a doctor that the surgery to fix it generally has a poor outcome and that I should just stop running.
The strange thing for me was that I noticed I rarely had symptoms playing soccer in flat, hard soled cleats, but only when running in running shoes. So I spent a couple years changing from a heel strike to a mid foot strike and do all my running in either minimalist shoes (now that they exist) or racing flats. At 45, my milage and times are better than ever. HOWEVER… for the last month, the pain in my right heel has been coming back and I can see the hand writing on the wall.
I don’t have the answers, but over the long term this seems to be something that can “come and go.” And I am definitely thinking about giving the Hokas a try soon.
Hey Pete,
Sorry to hear this. I know a bit about this and got it under control years ago but I had to do several things and accept some limitations in terms of the percentage of barefoot and true minimalist running I incorporated on a weekly basis. Feel free to contact me directly and I’ll share more if you are interested.
Harry
Harry,
Could you give me an idea of how you treated this problem. Would be grateful for some tips.
I have had moderate pain in my left heel right at the insertion point for approximately three months.
Thanks.
— Rob
rsforster1@gmail.com
Allan:
You are experiencing a fairly typical injury that I often see in my sports podiatry practice: retrocalcaneal bursitis. This injury seems to occur mostly in runners over the age of 40 and is a result of inflammation of a bursa that exists between the front (i.e. anterior aspect) of the Achilles tendon and the back (i.e. posterior aspect) of the calcaneus, basically sandwiched tightly between the Achilles tendon and the posterior calcaneus. This injury is commonly misdiagnosed as “Achilles tendinitis” when, in fact, it is the bursa itself which is causing the pain and swelling (i.e. edema). It may or may not be associated with a retrocalcaneal spur, which, by the way, you do not have on your x-rays (i.e. standing lateral radiograph of the foot). However, you do have quite a prominent posterior-superior prominence to the calcaneus which may be one of the reasons why you developed retrocalcaneal bursitis, including your transition to shoe with a lower heel (i.e. lower heel-height differential) prior to your injury developing.
A few months ago, I had two of the best over-40 distance runners in my area in my office with retrocalcaneal bursitis which was limiting their training. Here is what helped them.
First of all, at all times, you need to wear a running shoe with a heel lift so that the combination of heel-height differential from the shoe and heel lift inside the shoe, combined, is at least 15 mm. Typically, for a traditional, non-minimalist style, running shoe, this will mean using a ¼” (6 mm) neoprene heel lift inside the running shoe, under the heel of the sockliner of the shoe. This running shoe modification will decrease the tensile force on the Achilles tendon and rotate the posterior calcaneus away from Achilles tendon so that the Achilles tendon will exert less compression force on the retrocalcaneal bursa against the posterior calcaneus with each running step.
Second, I will have the runners actually take a scissor and knife and cut out the posterior heel counter of their running shoe so there is absolutely no compression or shearing force between the heel counter of the shoe and the posterior aspect of the heel during running. This running shoe modification will decrease the irritation to the retrocalcaneal bursa by decreasing the retrocalcaneal compression force at the running shoe-foot interface. Leave about ¼” of superior heel counter fabric at the top of the heel counter so that the shoe will still stay on the foot while running.
Third, you should avoid walking or standing barefoot or in any low heeled shoes with a firm heel counter while the bursitis is painful and swollen. Many patients have found great relief from this injury by switching their walking shoe to a clog (Dansko makes a number of very popular clogs) that has no heel counter (i.e. open back shoe). The Crocs sandal also makes an excellent cushioned open backed clog for walking around the house. I even have a number of patients (non-runners) with this condition that I have put into the open-backed Z-coil shoe, which has a large spring in the heel, and swear by this shoe for relief of retrocalcaneal bursitis. The reason for the need to change your walking shoes and around-the-house shoes is that even walking and standing in a shoe with a lowered heel and heel counter that compresses the retrocalcaneal bursa throughout the day will increase the inflammation within the bursa sufficiently to cause the injury to become chronic and not heal.
Fourth, I have also recently been using a relatively new prescription topical medicine that seems to be working quite well for retrocalcaneal bursitis. This is Voltaren gel, and is a topical prescription anti-inflammatory medicine that we have used for years as an oral non-steroidal anti-inflammatory drug and has now been formulated into a gel that can be absorbed through the skin and into the surrounding, deeper soft tissues. I have my patients apply the Voltaren gel three times a day to the posterior heel as long as the inflammation persists. You will need to have your physician prescribe this medicine for you, or maybe your foot doctor has a sample of it in his office you can try to see if it works. Of course, icing therapy, 20 minutes twice a day to the posterior heel is a standard treatment also for this injury.
You may find that there is a certain minimal heel height differential in your running shoe that you will be able to tolerate before you start experiencing symptoms again. Start out with a traditional running shoe with a 6 mm heel lift added inside the shoe, then reduce the heel lift, after the symptoms vanish, no more than 3 mm every 2 weeks to see how your heel responds to the return to less heel elevation when you run. Unfortunately, due to peculiar anatomy of your posterior heel, you will not likely ever be able to return to running full time in a low heel-height differential shoe. In addition, I would avoid surgery on this until all possible conservative measures have been exhausted since surgery for this is not always successful and can cause painful post-surgical scarring which would also limit your running.
Hope this helps you return to your running with less pain and more enjoyment.
Kevin A. Kirby, DPM
Adjunct Associate Professor
Department of Applied Biomechanics
California School of Podiatric Medicine
Private Practice:
107 Scripps Drive, Suite 200
Sacramento, CA 95825 USA
Kevin,
Thanks for your thoughtful input, I agree with everything you say here. If a conservative approach is preferred, I think this is absolutely a case where a heel lift is warranted and in fact probably essential, and I like your suggestion of starting high and slowly stepping down the lift based on individual tolerance. The key seems to be minimizing rubbing between the bursa and calcaneus, and changing the angle between the tendon and bone via a heel lift makes perfect sense.
Question for you – what causes Haglund’s to form? Some seem to indicate a genetic component, others indicate friction with a stiff heel counter stimulating bone deposition. For example, got an email from a sports med doc who indicated that he frequently sees it in hockey players due to chronic use of skates.
Pete
Pete:
There are plenty of osseous deformities of the posterior heel that can cause posterior heel pain. Haglund’s deformity, first described in 1928 by Haglund (of course), is an abnormal prominence of the posterior-superior-lateral heel that can cause posterior heel pain, especially in tight heel counter shoes or sports (e.g. ice skating) link to books.google.com?… These deformities sometimes need to be treated surgically, but, in my experience, the deformities can be treated successfully conservatively with the treatment techniques I described earlier.
As far as how they are formed, they can be caused by genetics, with individuals with a higher arched foot than normal (i.e. pes cavus deformity) having a higher calcaneal inclination angle which can increase the prominence of the posterior-superior calcaneus (which seems to be some of the problem with Allan’s foot). We also think these posterior heel prominences/exostoses can grow with chronic compression and tension stresses on the bone, but we aren’t sure why some people grow such large ones while others don’t.
The other variant that nearly always requires surgery are those individuals with a large Achilles tendon insertional calcification where there is a sharp dropoff (i.e. osseous shelf) where the Achilles tendon inserts. These seem to more likely require surgery but, in the patients I have treated surgically, seem to do much better post-surgically due to the removal of this sharp bony shelf that likely reduces the irritation to the Achilles tendon.
Cheers,
Kevin
Thanks Dr. Kirby. I’m hoping to return to running without surgery. I figure I’ve run 7 marathons and have probably had this haglunds for most of them so I can probably get back healthy again.
I’m having trouble believing that the pressure of the heel counter could cause the growth of the haglunds. The force of that compared to the other forces applied to the heel bone by the ground and the achilles seems neglible. I can believe that it could irritate the bursa and other soft tissue, but not that it could stimulate the bone growth.
Hi Kevin
I am a 41 year old sprinter suffering from achilles bursitis, and found your post very useful.
The only thing that was unclear (I may have missed it) was whether your patients are actually running in their modified shoes (with heel counters cut out)?
I have had the condition for four weeks, and iced and used ibuprofen gel regularly for the first two. The inflammation and pain has reduced dramatically, but I can still feel it first thing in the morning when I get up. I have not trained at all as I have had tonsillitis and a chest infection at the same time. I did do calf stretches for a week or so, but then wondered if they were aggravating the bursa.
I have not been wearing heel lifts, but am going to give it a try. My question is, are you advocating that your running patients return to training using the modified shoes BEFORE the condition has cleared up 100%?
My gut feeling is that if I can still feel the condition (albeit only slightly) when walking, won’t a return to jogging or sprint training just re-aggravate the injury, even using heel lifts? And won’t that slow down the overall recovery?
I’ve been using minimalist shoes for more than a year and had adjusted to having no heel differential, but was doing calf stretches for several months before the injury to overcome tightness and improve dorsiflexion and ankle mobility.
Is active recovery the way to go, or should I wait until I am symptom free?
Thanks in advance for your advice.
I’ve been experiencing symptoms of Retrocalcaneal bursitis recently as well. Pain on the very bottom/back of the foot, just below the Achilles. It hurts in the morning when I wake up, but gets slightly better through the day. I can actually run on it pretty good, the pain subsides, but then it just never gets better, I’m almost always hobbled the next morning.
I currently run in Newton Gravitas Trainers. I’ve been running in them for almost a year now, but haven’t experienced these symptoms until the last month. I also wear custom orthotics, so they add some to the heel/toe drop of the Newtons. I don’t know exactly, but they are certainly a few mm above the normal 4.
I have a million cause/correlation scenarios, and really no way to determine what will help beyond crude trial and error. Too much mileage on my Newtons? Do I need new shoes? Different model? New orthotics? No orthotics? Additional heel lift? More rest? Stretch/no stretch? Very frustrating. This and I have come off of a year long ordeal with ITBS has almost got me to quit running altogether.
Sounds more like insertional tendonitis than bursitis. I have had both. FWIW, several months of stretching really has helped some, but hasn’t completely resolved the symptoms. I’m currently trying out the rehab recommended in the following link:
http://runningwritings.blogspo…
It seems to be doing a good job of targeting the affected area. Will have to see how it does at remodeling the tendon an resolving the issue. The good news is that it doesn’t seem to be causing the bursitis to flair up.
Cool, thanks for the link. I’ll try the flat eccentric heel drops. Basically it’s just like a heel drop, except you do it on the flat floor instead of a step?
I have the exact same symptoms right now. Please post back if you find something that works. Thanks.
I have never been a runner, but I love to walk. After total knee replacement in 2009, which is going to have to be revised, I never got back to my former ability. I have wore athletic shoes purchased at a store in which the employee videos your stride, watches you walk and stand on your toes, etc since I had torn cartiledge removed in 1997. After this evaluation, the employee, usually a college grad with a degree in sports injuries, etc, then recommends the best type shoe for you, with about 5 brands to choose from. (BTW, I’ve never seen a Nike in any of these type stores.)
After all those commercials on TV touting the Skechers ‘Shape ups’, I decided to try them. I sent back the pair I ordered b/c I just thought they made my foot feel unnatural in a walk down the hall. But months later, when I LOST my (new) good walking shoes (I suspect they fell off the roof of my car – don’t ask), I bought the Asics brand of the ‘Shape ups’ type shoes at a generic shoe store. I wore them for just over a year, and walked in them almost every day. Never did feel exactly right, but I kept thinking how they’d build up my calves and gluts, according to the commercials!
Meanwhile, I need to mention that after the TKR surgery, I wore flat shoes 90% of the time. I noticed that my feet sort of hurt and that my calf muscles felt tight when I wore them or when I went barefoot after taking the flats off.
Back to the present: I started having more painful foot problems in both feet last summer. Then, out of the blue, I saw I had these awful looking protrusions on the backs of both heels. I went to an orthopedist to decide about my TKR revision and asked him what those outgrowths were. He took x-rays and said ‘Insertional Haglund’s Achilles Tendinitis’. Not wanting to go the conservative route of ‘resting’ the pumpbumps in a walking cast for 12 weeks+ because ‘it would not get rid of the protrusions on my heels”, I went to a podiatrist who was willing to do the surgery. That was Aug 15, 2011. It’s now 5 months later and I cannot yet wear anything but my New Balance (with inserts which the podiatrist added). How beautiful! Did I mention that I am a woman? I wore the boot cast for 3-4 months, gradually switching over to the NB’s. Every night, the back of my surgical heel is swollen. I’ve been going to PT, now 2x a week, but nothing seems to help. I am soooo sick of not being able to walk! I used to walk my dog at least 1-2 miles a day. I walked 1/4 mile recently and the PT thinks that set me back considerably!!
After reading of all these other experiences runners have had, I’m convinced that those stupid (ought to be illegal) ‘shape ups’ caused this problem! [And that shoes have been the culprit in most of the runners’ cases.] Just think about how far they (shape ups) stretch the tendon as your heel goes down much farther than is natural. Both the orthopedist and the podiatrist ‘don’t disagree’ with my thinking the shoes caused my HIAT. All I know is I want to get done with this. I cannot recommend the surgery. It really didn’t get rid of the bump, not all of it. Now it’s sort of over to the outside of the back of the heel, even after having the calcification cleaned up some in my tendon and the bone in the bottom of my foot cut and a piece taken out so the bones would knit back together.Let me tell you, foot surgery is horrible! BUT… I think if I have to have it redone, I’d have an orthopedist specialist (ft/ankle) do it, since they are trained medical doctors/surgeons. I didn’t know that podiatrists weren’t, and I’m sure most of them do wonderful work and help thousands with treatments and have even done this surgery successful. But I’m just kind of skittish now.
The idea of having my alignment evaluated, probably by a chiropractor, and getting some adjustments as well as a few of the other new treatments I’ve seen on this blog really sounds like the way to go. Any suggestions?
Linda
I’m suffering from the same type of heel pain; I believe mine started after trying to change to a midfoot landing instead of heel striking. I’ve run several marathons and have never been injured before. I’ve been to numerous physicians, tried PT, cortisone dose packs, stretching and heel drop exercises all to no avail. The best pain relief I’ve experienced so far has been as a result of weekly massages for the past 2 months. I’m going to try the flat foot heel raises since I got no relief from the others. Thanks for the info. I realize it has been several months since this post; assume you must be better? I’ve been battling this injury for 2 years and can only walk/run 2-3 miles after all this time and that has only been since I started the weekly massage. But I’m grateful for that because for months it was difficult to walk at all.
You massage the swollen area on the heel? I can’t decide if that’s a good decision or not. Massaging cramped calves (especially with ice) is great for breaking up scar tissue and fixing that problem. But I don’t know if this is the same thing. Someone else mentioned Graston’s technique, which seems similar. Is that what you do?
Just a follow up. My heel never healed up and I went back to the doctor who got an MRI that showed bad bursitis, tendonosis, a groove being worn in the tendon by the Haglunds, and a partial tear in the tendon. I had surgery on February 2 and had the Haglunds and bursa removed and the tendon debrided with about 50% of the attachment detached and then reattached. I have to say that this is a fairly nasty procedure to recovery from with the projected full recovery time being 6 to 9 months. In the meantime it has been a slow a painful rehab to get back walking and I’m just now starting to jog a few steps at the end of my walks. But things continue to improve steadily and I’m hopeful to be back to light running by the end of the summer.
Allan- very curious on how your surgery and ultimate recovery went? Were you able to return to your normal running? Any problems? I have been suffering through all the same problems for over 15 years. My last conservative approach before surgery.
Can anyone else tell me about their experience with surgery for these problems.
I, for the same reasons, am trying to transition to Vibram’s due to hip soreness. I have noticed that when I run barefoot that the pain in my hip is virtually completely gone. Now my weight is around 215lb and my transition has been long. I jhave the same pain you described in your blog (Allan). Since mid-dec 2011 I have been transitioning into barefoot running. To make a long story short, I have been laid up in between run for 1 -3 weeks to recover from calf and achilles tendons soreness. Although the strength in my calves and tendons have been getting much stronger, I need to give more time in between barefoot runs. Since running barefoot (Vibram) on treadmills seem to be an easier and less painful way to transition, I will continue with my barefoot running on the treadmill and regular running shoe running on the street. (10k, 12k, half\full marathon)
I have the same problem. No problems ever with traditional heel strike running (except for bad calf cramps from time to time that seem to be corrected by increased potassium). Then I got Saucony Hattoris (no heel lift at all), love them and felt really good building up my ankle muscles with a forefoot strike. Then a bump at the insertion point of my left heel. Don’t know why or when it came. No specific injury. But there is a sharp pain a little to the outside of the heel bump. Feels like a small tear almost. And I’ve been icing and laying off it for months but it won’t heal.
That said, I walk around at home barefoot and I wear flip flops all the time. And I have shoes without heel lift, and it does feel sore when I walk in them a lot. And Ashtanga yoga, which I do a lot now, also probably doesn’t help…standing and balance poses will make it more sore afterwards if my form isn’t perfect and I put a little too much stress on that ankle. So I guess the key is creating a heel lift to give it a break and some time to heal.
I guess I’m going to go back to my traditional Brooks Adrenalines and my old heel foot strike. Barefoot running is great in theory and feels a slight bit better on my lower back, but it’s not worth risking chronic injury, you know? Plus, I do yoga to correct my posture. I run to stay in aerobic shape.
Also, I know I don’t have perfect form. My hips are tight, my IT band is tight, my psoas is tight, that’s why Ashtanga is great to work on those things. But it’s going to take a long time to correct those things. And I do have a pretty good barefoot technique: forefoot strike, light impact, shorter strides…everything was working out great with the barefoot running. I feel like Allan’s conclusion about this injury is the best one I’ve heard.
Hi allan,
I am a very atheletic person , male , 35 years. On october 9, 2011 while playing badminton , I endured a complete rupture of my achilles tendon at about 4-5 inches above the ground height. I went thru surgery on 15 Oct. and my leg (right) was placed in a cast for 3 weeks after which my surgeon removed the cast and changed the angle of my foot and placed the cast back for another 3 weeks , so total 6 weeks in a cast . Subsequently I started physiotherapy , lots of stretching etc, for about 2 months during which I started walking and after about 1 and a half month from the time the cast came off I was able to run , but I consciously did so at a slow speed not to damage anything . I did this for about 2 weeks and then completely stopped running for about 2 months because I couldnt take time off for sport due to other commitments . However from the time I first started running I have been experiencing pain on the posterior part of my heel bone which spreads to the inner side of the heel bone .This happens when my heel lifts off the ground while running , basically when I bear weight . But this pain does not come when I walk .Its only when because of running when more force is applied on the ground that the pain starts . Also If i sit in a place for long and get up , there is pain for the first 10-15 steps ,then it settles down and no pain while walking but, if I start to run , like I explained earlier the pain starts again.What do you think is the problem and what can I do to sort it out. I have started my running again since the last 3 months , I run an average of 4-5 kms everytime but with pain.Could you please email me on my id cpl_y2k@hotmail.com . Thanks – Sid.
Hi allan,
I am a very atheletic person , male , 35 years. On october 9, 2011 while playing badminton , I endured a complete rupture of my achilles tendon at about 4-5 inches above the ground height. I went thru surgery on 15 Oct. and my leg (right) was placed in a cast for 3 weeks after which my surgeon removed the cast and changed the angle of my foot and placed the cast back for another 3 weeks , so total 6 weeks in a cast . Subsequently I started physiotherapy , lots of stretching etc, for about 2 months during which I started walking and after about 1 and a half month from the time the cast came off I was able to run , but I consciously did so at a slow speed not to damage anything . I did this for about 2 weeks and then completely stopped running for about 2 months because I couldnt take time off for sport due to other commitments . However from the time I first started running I have been experiencing pain on the posterior part of my heel bone which spreads to the inner side of the heel bone .This happens when my heel lifts off the ground while running , basically when I bear weight . But this pain does not come when I walk .Its only when because of running when more force is applied on the ground that the pain starts . Also If i sit in a place for long and get up , there is pain for the first 10-15 steps ,then it settles down and no pain while walking but, if I start to run , like I explained earlier the pain starts again.What do you think is the problem and what can I do to sort it out. I have started my running again since the last 3 months , I run an average of 4-5 kms everytime but with pain.Could you please email me on my id cpl_y2k@hotmail.com . Thanks – Sid.
Hi I found the article sub posted within this comments section to be extremely helpful. I have had AT before and was exposed to the eccentric heel drop . Naturally i tried to do the heel drop off a step when i had insertional achilles tendinopathy. Now I know that it must be done on flat surface. Has anyone further investigated the use of the flat surface regimen for Insertional Achilles tendinopathy?
Hi, Thanks for the article. It is very informative. I am 25 years old and have flat feet. I have been using arches in my shoes since 4 years as I got pain in my toes with walking. I donot run but I have been suffering from similar pain as in insertional achilles tendonitis since a month in left ankle. The pain is only felt while moving downstairs. I have no issue while walking. But if I use stairs many times I get a constant pain but no swelling. Dr. suggested my NSAIDs and a gel with 0.5% piroxicam and told me to take rest. It has been 15 days and I feel no improvement. I will perform the heel down exercise as described above but i feel no pain while doing it so should i directly use a back pack? Plus can I start with brisk walk which I have left after visiting my doctor who suggested rest? Is my condition tendonitis or am I confusing it with other conditions? I am in a great depression due to this. Cannot go down steps with putting stress on my left foot. Will I be able to step downstairs normal again?
Is there any other exercise that I should do? like stretching with a towel? Despirately waiting for your reply. Thanks
Is there any difference in pain level when walking down stairs barefoot vs. in your typical shoes? Also, what shoes do you wear? Sometimes a shoe with a hard backing behind the heel can exacerbate pain at the Achilles insertion.
Hi Peter,
I know this discussion is pretty old, but I figured I would chime in with my experience. I’m no athlete. I’m a 31 year old woman who works at a hospital and stands or walks for most of the the work day. One evening about two weeks ago I was getting my things together before leaving work. I took a step and felt/heard a loud pop. You can guess what happened; I ruptured my Achilles’ tendon.
My ortho was puzzled about how this happened, since I was not engaged in any strenuous physical activity. Even an MRI yielded few answers, though it did show Haglund’s deformity (and, also, he could tell that just from looking at my heel). During surgery to repair this mess of an injury, it all became clear. The Haglund’s contributed to bursitis and insertional tendinitis. My Achilles, in fact, had become so degenerated that 40% of it had separated from my calcaneus entirely. The remaining 60% was not strong enough to hold, so it ruptured higher up. He he had to do a complicated re attachment and repair, which involved shaving down the Haglund’s, screwing the tendon back into the calcaneus, repairing higher up, etc.
In short, I will *never* wear a shoe again that is not Achilles supportive. I was wearing a lot of Sanuks, Tom’s, flat Merrill’s, etc. This ordeal has been a nightmare, and I’m very invested in protecting my Achilles at all costs! I’m wearing one ASICs Kayano right now. Can’t wait to put the other one on when this ortho boot comes off in 12 weeks.